Wound healing is a complex and intricate process involving physiological events to repair damaged tissue and restore normal function. However, for individuals with diabetes, this natural therapeutic process can become compromised, leading to the development of chronic wounds and complications such as arterial leg ulcers and venous ulcers.
Arterial leg ulcers primarily arise from peripheral arterial disease (PAD), a condition characterized by the narrowing or blockage of arteries that supply blood to the legs. The most common cause of PAD is atherosclerosis, a buildup of fatty deposits within the arterial walls. Other factors contributing to arterial leg ulcers include diabetes, smoking, hypertension, and a sedentary lifestyle.
Diagnosis:
Proper diagnosis of arterial leg ulcers involves a thorough examination by a healthcare professional. It may include a detailed medical history, physical examination, and diagnostic tests such as Doppler ultrasound, ankle-brachial index (ABI) measurement, and angiography. These tests help determine the extent of arterial blockage and guide the development of an appropriate treatment plan.
Chronic Wounds, a combination of factors
Chronic wound fails to progress through the normal stages of healing in a timely and organized manner. In individuals with diabetes, chronic injuries often result from a combination of factors, including poor blood circulation, peripheral neuropathy (nerve damage), and compromised immune function. The impaired ability to sense pain and pressure due to neuropathy can lead to unnoticed injuries, allowing wounds to progress to chronic stages.
Arterial Leg Ulcers:
Arterial leg ulcers are a specific chronic wound commonly associated with diabetes. These ulcers result from inadequate blood supply to the lower extremities, a condition known as peripheral arterial disease (PAD). In diabetes, high glucose levels can contribute to the formation of atherosclerotic plaques in the arteries, further restricting blood flow. The lack of oxygen and nutrients reaching the tissues in the legs can lead to the development of ulcers, particularly in areas that experience constant pressure or trauma.
Venous Ulcers:
Venous ulcer is more prevalent in individuals with diabetes who also suffer from venous insufficiency. Venous insufficiency occurs when the veins in the legs fail to efficiently return blood to the heart, causing blood to pool in the lower extremities. This stagnant blood can lead to inflammation, skin changes, and venous ulcers. In diabetes, impaired blood flow and compromised tissue repair mechanisms significantly increase the risk of venous ulcer formation.
Venous ulcer is more prevalent in individuals with diabetes who also suffer from venous insufficiency.
Challenges in Diabetic Wound Healing:
Several factors contribute to the challenges associated with wound healing in individuals with diabetes. Firstly, hyperglycemia, or high blood sugar levels, can impair the function of immune cells, reducing the body's ability to fend off infections at the wound site. Additionally, the compromised blood flow in diabetes limits the delivery of essential nutrients and oxygen to the wound, further hindering the healing process.
Furthermore, the presence of neuropathy in diabetes can mask pain sensations, leading to delayed detection of wounds and allowing them to progress to more advanced stages. This delayed recognition exacerbates the difficulty of managing chronic wounds effectively.
Management and Prevention:
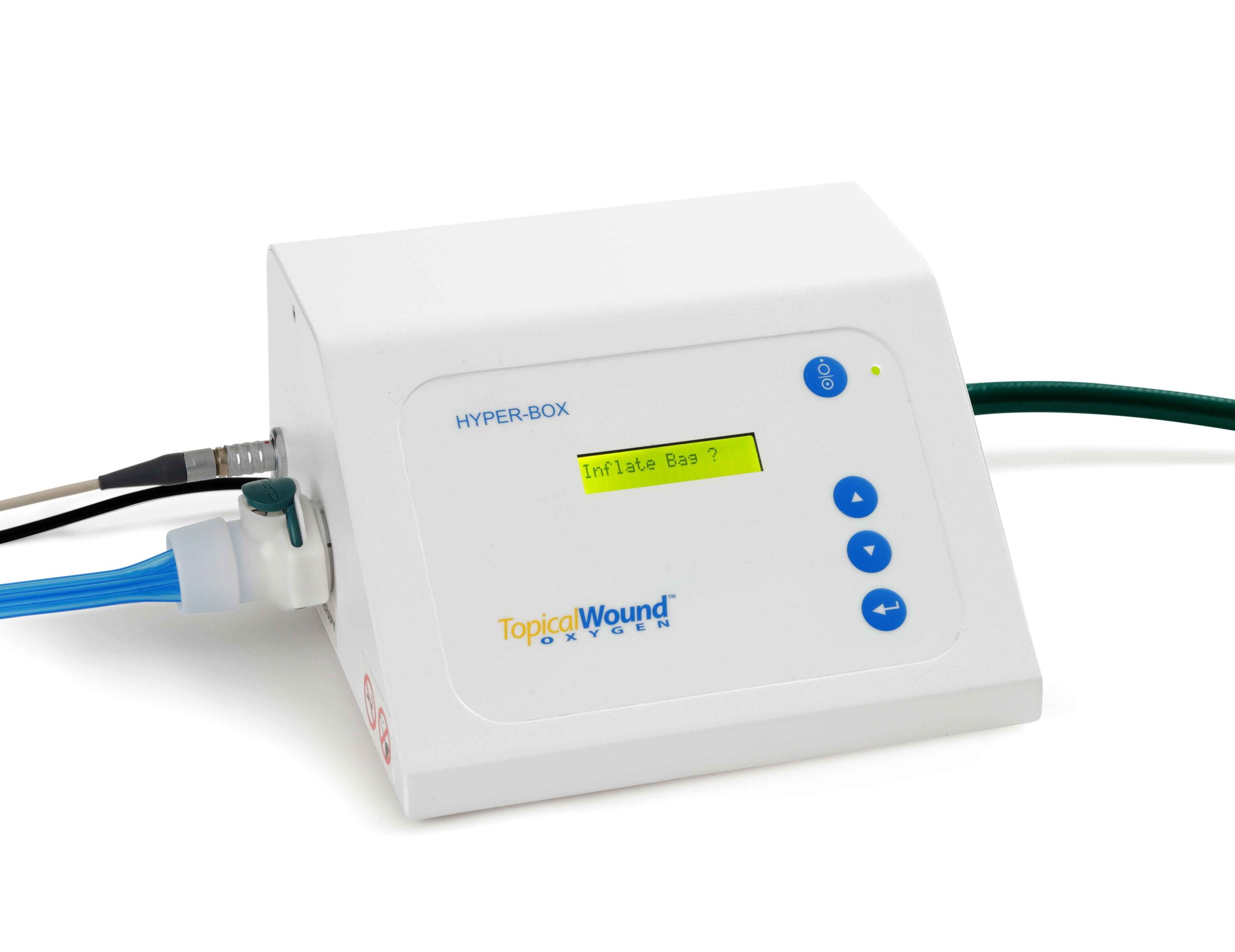
The management of wound healing and diabetes require a multidisciplinary approach. This may include controlling blood glucose levels, improving blood circulation through medications or surgical interventions, and implementing advanced wound care techniques.
Prevention plays a crucial role in minimizing the risk of chronic wounds. Regular foot care, including inspection for cuts or injuries, proper footwear, and maintaining healthy blood sugar levels, can help prevent the development of diabetic foot ulcers. Additionally, lifestyle modifications such as smoking cessation and maintaining a healthy diet contribute to overall vascular health, reducing the risk of arterial and venous ulcers.
Conclusion:
The interplay between diabetes and wound healing is a complex and multifaceted relationship. Chronic wounds, arterial leg ulcers, and venous ulcers pose significant challenges for individuals with diabetes, necessitating comprehensive management strategies. As our understanding of the underlying mechanisms continues to evolve, ongoing research and advancements in treatment modalities offer hope for improved outcomes and a better quality of life for those affected by this intricate interplay of metabolic and wound-healing processes.
For more information about wound healing and diabetes, click here to Advanced Oxygen Therapy Inc. for the best wound care or healing programs.





